Dermatologist Guide to Psoriasis, Preventing Flares, and New Treatments
What Is Psoriasis?
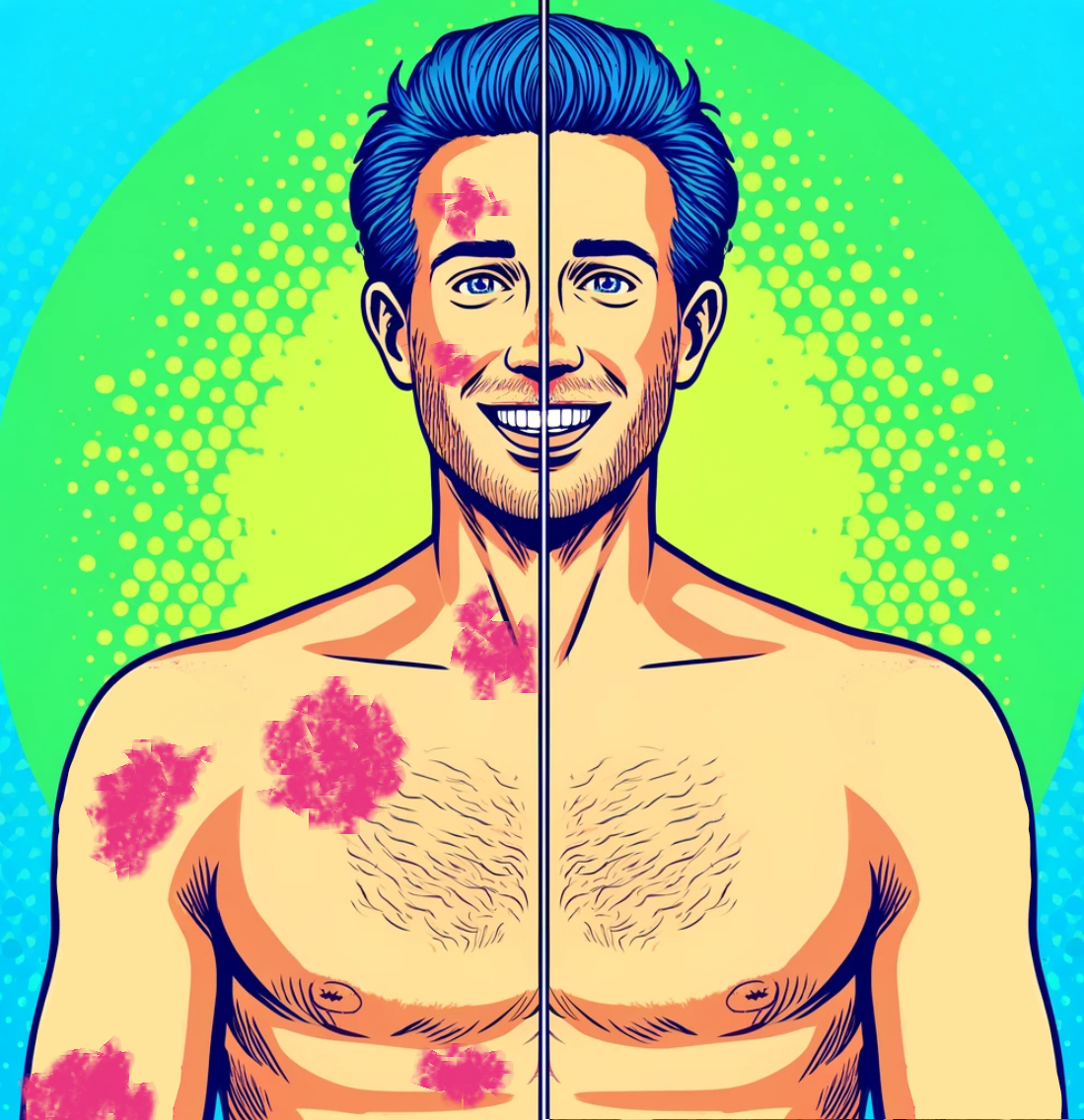
Psoriasis is a common skin condition that causes skin inflammation and rapid turnover of skin cells. Normally, it takes about a month for new skin cells to rise to the surface. With psoriasis, this process only takes about 3-4 days, causing a buildup of skin cells that form raised, red, scaly plaques on the skin. While the condition may come and go, it most often develops into a chronic lifelong disease needing long-term management.
Different Types of Psoriasis
There are several forms of psoriasis ranging in severity. The most common type is plaque psoriasis. Others include guttate, inverse, pustular, and erythrodermic psoriasis.
Plaque Psoriasis
Plaque psoriasis causes dry, raised, red skin lesions (plaques) covered with silvery scales. Plaques commonly develop on elbows, knees, scalp and lower back but can appear anywhere. Plaque psoriasis accounts for about 80-90% cases, making it the most prevalent form.
Symptoms: dry, raised, red plaques covered in silver-white scales appearing on common areas like elbows and knees or across large swaths of skin. Plaques can crack and bleed in severe cases.
Guttate Psoriasis
Guttate psoriasis triggers small, water-drop shaped sores on the skin. Often starts in childhood or young adulthood soon after a bacterial infections like strep throat. Tend to resolve after a few weeks to months but some eventually develop plaque psoriasis over time. About 10% of people with psoriasis have guttate lesions.
Symptoms: multiple small, salmon-pink bumps primarily on the trunk arms, legs and scalp. Sometimes fine scales with lower tendency to thicken. Often appears suddenly and can resolve on its own or develop into plaque psoriasis.
Inverse Psoriasis
Inverse psoriasis causes bright red, shiny lesions without scales in skin folds like genitals, buttocks, underarms, under breasts. Skin-on-skin friction and sweating make this form show up in sensitive areas unlike other types triggered at points of drying and irritation. About 3-7% of psoriasis is inverse.
Symptoms: smooth, bright red lesions typically lacking scales in body folds that can worsen with friction and sweating. Inverse psoriasis does not typically itch like other forms but can cause irritation, pain and bleeding cracks due to location in tender areas.
Pustular Psoriasis
Pustular psoriasis is an uncommon, severe variety causing pus-filled blisters rather than plaques. Comes in localized form with pustules limited to hands and feet or generalized form covering most of the body. Flare-ups tend to cycle in and out acutely.
Symptoms: Studding of the skin with swollen pustules surrounded by inflamed, irritated skin. Tendency for cycles of flares over days alternated with remission periods. Fever, chills, severe itching, exhaustion, an accelerated heart rate and other signs of instability and infection. Requires close supervision by a dermatologist for this form of psoriasis.
Erythrodermic Psoriasis
Erythodermic psoriasis produces severe inflammation and shedding affecting most of the body, which can disrupt thermoregulation. Without treatment, it can become life-threatening. Causes protein and fluid loss leading to infection, pneumonia or congestive heart failure. Requires emergency treatment.
Symptoms: intense shedding and inflammation making skin look intensely red and raw resembling a severe burn. Can cause fevers, chills, rapid pulse, pain, itching and body temperature dysregulation from compromised protective skin barrier necessitating urgent medical intervention.
What Causes Psoriasis?
The exact cause remains unknown, but it’s an immune-mediated condition. A combination of genetics, immune system functioning and environmental exposures like infections is thought to activate abnormal immune responses causing uncontrolled turnover of skin cells and inflammation.
Common triggers include:
Infections like strep throat activating an excessive immune reaction
Stress causing flare-ups in over 50% of patients
Skin injuries, sunburns or irritants disrupting skin barrier
While not contagious from person-to-person, family history plays a role. Those with a first-degree relative with the disease have about 50% higher chance of developing psoriasis themselves.
Psoriatic Arthritis
Around 30% of psoriasis patients eventually get psoriatic arthritis - which causes swollen, painful joints leading to permanent damage over time. It shares a common underlying autoimmune cause with psoriasis meaning managing skin disease remains key to prevent future debilitating arthritis.
Symptoms include:
Swelling, pain and stiffness in joints often in asymmetric patterns
Reduced range of motion, stiffness especially early morning
Nail changes - pits and grooves
Eye problems like conjunctivitis
Consult a rheumatologist promptly if you experience these to prevent irreversible joint destruction and immobility through early treatment.
Diagnosing Psoriasis
Getting properly diagnosed allows you to create an effective treatment plan targeting your specific type and pattern of psoriasis. When you see a dermatologist, they will typically take a medical history examining symptom timelines, triggers, past treatments tried and family history of psoriasis or autoimmune diseases.
They may conduct a skin examination evaluating lesions in terms of:
Location – Where are plaques located on your body? This can differentiate types like inverse or plaque.
Appearance – What do psoriatic lesions look like? Assessing color, thickness, dryness, and scales patterns can indicate severity.
Percentage of body covered – What percent of skin surface contains plaque buildup? Mild cases have less than 3% involvement while severe is over 10%.
Dermatologists may also take a skin biopsy of lesion samples to rule out mimickers of psoriasis. No single test confirms psoriasis but examining presenting signs and symptoms along with ruling out differentials leads to an accurate determination. Blood tests check for genes and markers supporting a psoriasis diagnosis as well.
Psoriasis Severity
Assessing severity allows customized approaches targeting mild, moderate or advanced disease through graduated measures adjusted based on efficacy and control achieved.
Dermatologists classify mild, moderate and severe forms counting all skin surfaces involved by plaque measuring handprint size or greater.
Mild: Less than 3% of skin impacted Moderate: Between 3-10% of skin covered Severe: Over 10% body surface area impacted
More specific scales like PASI scoring calculate intensity of lesions multiplying by percentage of affected areas. Your dermatologist tailors treatment strategies to your severity score with periodic adjustments as needed.
Treating Psoriasis and New Medications
While no cure exists, the range of treatments for psoriasis continues expanding greatly aiding management/prevention of flares and symptoms. Multiple modalities now exist supporting sufficient control allowing normal day-to-day life for a majority of sufferers. Discuss options fully with your dermatologist weighting goals, lifestyle needs and risks together finding your optimal regimen.
Topicals
Common first-line treatments for mild cases applied directly to plaques, topical therapies reduce inflammation and scaling, slow down cell turnover and can clear or minimize outbreaks in contained areas.
Types range from over-the-counter creams and ointments containing salicylic acid and coal tar for gentle exfoliation and soothing to prescription topical corticosteroids that reduce inflammation or vitamin D analogs slowing skin cell growth. Rotate amongst different medication classes to avoid resistance.
Topical prescriptions such as VTAMA (tapinarof) has also shown to be very effective in cases of limited psoriasis. This is a nonsteroid medication that we have seen successful patient outcomes with.
Phototherapy
Phototherapy uses ultraviolet light under medical supervision to treat moderate/severe cases. Oral psoralen tablets used alongside controlled UV light exposure can treat widespread surface involvement where topicals prove insufficient by themselves. However, long term use raises skin cancer risk needing prevention.
Home phototherapy can be another option, as in office phototherapy often requires a major logistical change to a person’s schedule, often requiring three times a week visits to the clinic for phototherapy.
Oral Systemic Medications
For those failing topical therapy alone, oral or injectable systemic drugs treat moderate-severe psoriasis through immune-targeting effects reducing widespread lesions and symptoms when used alone or combined with creams, light or biologics.
Oral options may include:
Methotrexate: Anti-inflammatory targeting overactive immune responses. Requires monitoring for liver toxicity with long term use.
Apremilast (Otezla): Oral phosphodiesterase 4 (PDE4) inhibitor specifically approved for psoriasis targeting inflammation causing rapid skin cell growth. Generally better tolerated than other oral systemics.
Acitretin: Derivative of vitamin A reining in rapid skin cell production. Mainly combined with phototherapy boosting results. Causes birth defects mandating contraception so not used alone in childbearing age groups.
Cyclosporine: Immunosuppressive drug typically used short term for rapid clearance in severe recalcitrant plaques. Kidney and blood pressure monitoring necessary.
Some of these oral drugs require lab testing intermittently assessing response and possible side effects needing review.
Biologic Injections / Infusions
Biologics revolutionized psoriasis treatment by specifically blocking overactive components of inflammation related to out-of-control skin cell turnover and scaling.
Targets: TNF-alpha, IL-17, IL-12/23 inflammatory mediators promoting psoriatic lesions
Main Types
Anti-TNF agents: Adalimumab, etanercept, infliximab
Anti-IL 12/23 agents: Ustekinumab,
Anti-IL 17 agents: Ixekizumab, brodalumab, secukinumab
Anti-IL 23 agents (newest): Risankizumab, guselkumab, tildrakizumab
Highly effective for most difficult-to-treat cases of plaque psoriasis and depending on the choice of biologic - psoriatic arthritis
Close medical guidance determines best biologic candidates and appropriate safety monitoring for those not well controlled on other therapies or with extensive disease significantly impacting quality of life.
Ways to Prevent Flareups of Psoriasis
Managing psoriasis flare-ups requires a multifaceted approach, focusing on both skin care and lifestyle adjustments.
One of the most important things you can do is maintain skin hydration to prevent dryness and cracking, which can worsen psoriasis symptoms. A high-quality moisturizer specifically formulated for sensitive and psoriatic skin, such as CeraVe Psoriasis Moisturizing Cream, can provide the necessary hydration and barrier protection. This cream contains ceramides and niacinamide, supporting skin's natural barrier and reducing redness and itching. It also contains salicylic acid to help reduce scale.
Another effective way to soothe psoriasis symptoms is the use of over-the-counter topicals containing coal tar, an ingredient known for reducing inflammation and scaling (source).
Additionally, incorporating omega-3 supplements into your daily regimen can have systemic anti-inflammatory effects beneficial for psoriasis management. Over time, we have discovered that psoriasis can be associated with metabolic syndrome and cardiovascular risk factors (source), so supplementing with fish oil can be beneficial for psoriasis and its associated risk factors (source).
Summary Of Key Things To Remember
Plaque psoriasis is the most common variety; guttate, inverse, erythrodermic, pustular represent rarer forms.
Flare triggers include infections, skin injuries, stress and irritants disrupting skin barrier.
Diagnosis involves examining physical signs/symptoms and ruling out alternative conditions via skin biopsy or blood tests.
Judging severity scores determines treatment choices starting mild then graduating approaches as needed.
Range of options now exist beyond just topicals including phototherapy, oral systemics and advanced biologics.
-
What are the symptoms of psoriasis?
Psoriasis is a skin condition that commonly manifests as red, scaly patches on the skin. It can also cause itching, burning, or soreness. In some cases, individuals with psoriasis may experience psoriatic arthritis, leading to joint pain and swelling.
How is psoriasis diagnosed and treated?
Diagnosis and treatment of psoriasis should be performed by a dermatologist or a healthcare professional with expertise in dermatology. The American Academy of Dermatology and the National Psoriasis Foundation offer guidelines of care for the management and treatment of psoriasis, which include various treatment options such as topical therapy, biologics, and other alternative medicine modalities for psoriasis severity measures.
What are the common types of psoriasis?
The common types of psoriasis include plaque psoriasis, guttate psoriasis, pustular psoriasis, and inverse psoriasis. Each type may present differently and require specific treatment options.
How does psoriasis affect different skin types?
Psoriasis can affect individuals of all skin types, including individuals with skin of color. It is important to consider the specific needs and challenges of managing psoriasis in individuals with varying skin tones.
What causes psoriasis to flare?
The exact cause of psoriasis flares is not fully understood, but triggers such as stress, infections, certain medications, and changes in weather may exacerbate psoriasis symptoms. Effective management of psoriasis includes identifying and avoiding triggers that can lead to flares.
What are the treatment options for nail psoriasis?
Treatment of nail psoriasis may involve topical therapy applied to the affected nails, but typically systemic treatments are better for nail psoriasis as topicals do not adequately address the root of the problem.
What is severe psoriasis?
Severe psoriasis refers to the condition when skin cells grow at an abnormally fast rate, leading to the development of thick, red, and often itchy patches on the skin. In some cases, psoriasis can also be associated with psoriatic arthritis.
What are the AAD-NPF guidelines of care?
AAD-NPF guidelines of care refer to the joint guidelines developed by the American Academy of Dermatology (AAD) and the National Psoriasis Foundation (NPF) for the diagnosis and management of psoriasis, including treatment of psoriasis with biologics, topical therapy, and other methods to improve psoriasis symptoms.
How is psoriasis usually treated?
Psoriasis usually involves a combination of treatment methods, including topical therapy applied to the skin, biologic medications, and other systemic treatments. In some cases, phototherapy may also be recommended to improve psoriasis.
What is considered moderate to severe psoriasis?
Moderate to severe psoriasis refers to the extent and severity of the condition, often characterized by widespread inflammation and redness, covering a larger body surface area. It may require more aggressive treatment approaches, such as biologic therapies or oral medications.
Is psoriasis contagious?
Psoriasis is not contagious. It is a chronic, non-infectious condition resulting from an overactive immune system and skin cell growth cycle. Hence, it cannot be transmitted from person to person through contact.
-
We are a group of dermatology residents and attending physicians based in Boston, MA. Our team of Ivy League-trained dermatologists is demystifying the cosmeceutical industry by offering unbiased, scientifically supported reviews of skincare products. We are extremely passionate about skincare and making it accessible to all through education. We value integrity, practicality, and inclusivity. No sponsorships were received for the products prior to testing; we feel strongly about providing un-biased reviews. After blogs are published, following the links in this blog post may result in commission.