Everything You Need to Know Before Surgical Excision for Skin Cancer by Dermatologists
By Michael Shaughnessy, MD and David G. Li, MD, MBA
Michael Shaughnessy is an incoming Mohs Micrographic Surgery Fellow at Oregon Health & Science University (OHSU). He is currently a resident at the Harvard Medical School Combined Dermatology Program.
David Li is a board-certified dermatologist in private practice in downtown Boston and the Founder of BDA. Previously he was a resident at the Harvard Medical School Combined Dermatology Program.
Table of Contents
What Happens During an Excision?
Detailed Steps Involved in Excision to Treat Skin Cancers
What Can I Expect After Surgery?
How Do I Care for the Wound After Surgery?
What are the Risks and Possible Complications?
If your dermatologist has recommended surgical excision to treat your skin cancer, you likely have questions about the procedure.
What is an excision? What are the risks of the procedure? What can I expect for at home care, and will I have stitches? Do I have other options for treatment?
This article will cover key details to know beforehand allowing you to feel prepared and more comfortable on the day of your procedure.
What is Surgical Excision?
Excision is a common, safe, and effective treatment for basal cell carcinoma (BCC), squamous cell carcinoma (SCC), and melanoma, in addition to other skin cancers. Your dermatologist may recommend the procedure after a skin biopsy confirms that you have a diagnosis of skin cancer. Or, excision could be the first step, if your dermatologist is worried that something on your skin is cancerous based on its appearance and location.
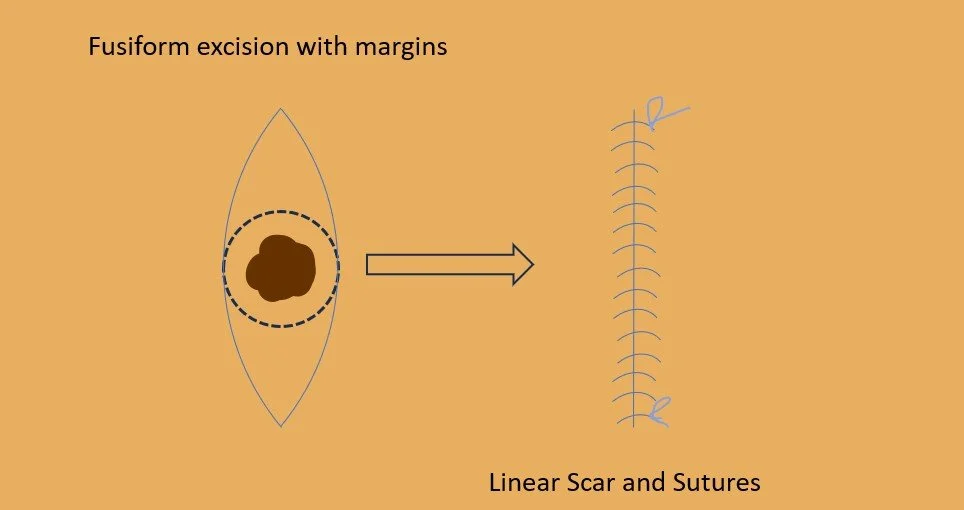
The goal of an excision is to surgically remove the entirety of your skin cancer along with a small rim of normal and healthy skin. Removal of this rim, or “margin”, ensures no cancer is left behind. Excision often leads to cure of your cancer, and your dermatologist will discuss the chance of successfully removing the cancer both before your procedure and after microscopic evaluation of the margin. In some cases, your dermatologist may recommend additional treatments to be completed before or after your procedure.
What Happens During an Excision?
An excision is typically performed right in your dermatologist’s office, and you remain awake during the whole outpatient procedure. Here’s a general overview:
After checking in on the day of your procedure, you will be brought into the procedure room and your dermatologist or their assistant will go over the procedure in detail and obtain your consent to proceeding.
The skin around the treatment area then gets cleaned and sterilized with alcohol, iodine, or other antibacterial solutions.
The area to be operated on gets numbed by injection of a local anesthetic so you don’t feel pain during the procedure. This is generally the only painful part of the procedure and is over in a minute or two.
Your dermatologist then outlines the tissue to be removed with a marker, which guides the removal and plan to close the skin.
Your dermatologist uses a scalpel, or sharp blade, to carefully cut around and underneath the cancer, which constitutes the “excision” or removal of the cancer from your skin.
Normal bleeding is stopped using electrical cautery or other techniques.
The excision is now complete, and closure or “reconstruction” of your wound begins.
In some cases, your wound will be left to heal on its own, but most of the time it will be closed with multiple layers of stitches, or “sutures” that allow for proper healing with minimal scarring.
A sterile bandage is applied to protect the site as it heals over the next few weeks. Your dermatologist or their assistant will then discuss how to take care of the wound at home.
The procedure typically takes between 30-45 minutes. Once finished, the excised sample gets sent to pathology to analyze the margin under a microscope and confirm the cancer was entirely removed.
Detailed Steps Involved in Excision to Treat Skin Cancers
Here are more detailed descriptions of the key components of the procedure:
Assessment and Consent
Your dermatologist will first thoroughly assess the suspicious lesion and decide if excision is the best treatment for you based on guidelines for various skin cancer types. Risk factors help guide management, and some cancers may be better treated with other approaches or alternatives.
If you and your dermatologist decide to proceed with the excision, he or she will properly go over the procedure, including the risks, benefits, and alternatives, to ensure you are informed and consent to the procedure.
They may also ask questions about your medical history, including the presence of any pacemakers or other electrical devices in your body, a history of heart disease, recent joint replacement, or the use of blood thinning medications, as these factors allow them to tailor the procedure to you. This is the best time to ask any questions you may have prior to beginning.
Outlining Margins
Using a surgical pen, your dermatologist then marks the ellipse (aka “football shape” or oval) of tissue to be excised, including the planned border, or margin, around the cancer. Sometimes the outlined plan can change during your procedure to ensure the cancer is fully removed and your wound has the highest chance of healing. Your dermatologist should inform you of any changes as they arise.
Anesthesia
Lidocaine or a similar numbing medication will then be injected into and under the skin to prevent any pain or discomfort during tissue removal. This is often one of the more uncomfortable parts of the entire procedure, as the numbing typically feels like an immediate pinch followed by a few seconds of an intense burning sensation. You shouldn’t feel sharp pain after this step, but may still experience pressure, pulling, or tugging.
Cancer Removal or Excision
A scalpel is used to precisely cut out the outlined section of tissue including the cancer itself and the margin of normal skin. The removal of the skin cancer, what your dermatologist terms the excision, is now complete, and techniques to address the resultant wound are undertaken. If there is high wound tension, then ‘undermining’ may also occur at this stage, which is when the surgeon separates some of the fibrous tissue around the surgical site to reduce the tension and improve the ability to fully close the wound.
Stopping Bleeding
Electrocautery (heat applied via localized electricity) quickly seals blood vessels that were damaged during the excision. Additional means like suture ties or cautery with various chemicals and solutions (chemical cautery) may also be used.
Wound Closure or “Reconstruction”
Your dermatologist will then explain options for treating the wound left by the excision. In most cases, the open wound will get closed using two layers (superficial and deep) of stitches or “sutures” to promote proper healing and minimize scarring. Often, this is done in a straight line and will result in a straight scar, but sometimes more complicated shapes or designs may be warranted depending on the size and location of the wound.
Bandaging or “Dressing”
Finally a sterile bandage or “dressing” gets placed over the site to keep it covered and clean while healing. Your bandage may be in a form familiar to you such as a Band-Aid, or could be a combination of gauze, tape, glue, or strips of tape called “Steri strips”. You will be provided with instructions on how to change this dressing and take care of the wound at home.
What Can I Expect After Surgery?
You may have temporary numbness at the excision site from the local anesthetic. This wears off over a few hours.
Mild discomfort, bruising or swelling at and around the site are normal. Over-the-counter medications such as Tylenol should be sufficient to treat this (some physicians may want you to avoid ibuprofen after the surgery as this can increase bleeding). Pain that is not treated by these medications or lasts longer than a few days should be reported to your dermatologist.
Your stitches will be removed in 1-2 weeks in most cases. At this point, your wound and scar will be healed but still swollen and pink or red.
Your dermatologist will report to you on final results of pathology on the excised cancer and margins within 1-2 weeks.
Follow wound care instructions from your doctor and expect healing to take place over 4-6 weeks.
Be diligent about sun protection, self-skin checks to monitor for new suspicious growths, and following up with your dermatologist for regular skin exams.
How Do I Care for the Wound After Surgery?
Keep the excision site covered with the dressing applied on the day of your procedure for as long as instructed, which may be anywhere from 1 day to 1 week.
Change the dressing as instructed, as often as every day or when visibly soiled.
Avoid getting the wound wet for as long as instructed, generally at least 1 day for a shower, but it may be longer depending on the extent of the procedure and will likely be longer for swimming in pools, ponds, lakes, or the ocean.
Your wound should be washed gently with warm water and soap as instructed and then gently pat to dry.
Wear loose comfortable clothing that doesn’t rub or put pressure on healing skin.
You may be asked to limit exercise and other strenuous activity at least until stitches are removed and sometimes longer.
Your dermatologist may discuss strategies to improve the appearance of your scar, such as the use of Vaseline, diligent sunscreen and sun protective measures, and silicone bandages.
What are the Risks and Possible Complications?
Infection: Rare (~1% or less in skin surgery). Your dermatologist will review what to watch for and prescribe antibiotics before, during, or after your surgery if necessary.
Abnormal scarring: Scars may thicken or become raised, discolored, or indented. In rare circumstances, you may be offered additional treatment to improve the scar’s appearance.
Recurrence: There is always a risk that your cancer comes back, and your dermatologist should discuss the likelihood of this along with strategies to prevent or monitor this.
Numbness: You may experience numbness around the procedure for months, years, or sometimes permanently due to nerve injury during your surgery.
Wound separation or “dehiscence”: It does not occur often, but sometimes the stitches can “pop” and your wound may open back up before completely healing. Your dermatologist should be informed immediately if this occurs.
Hematoma: A hematoma (or bleeding underneath the skin) can sometimes occur after surgery. Your dermatologist may warn you about what to watch for, including intense pain and a larger than normal swelling of your wound.
All of these complications are uncommon but can occur even when all portions of your procedure go as planned. It is important to ask what you can do to help prevent and look out for them and promptly consult your dermatologist if you have any questions or concerns.
Is there Anything I Can Do to Improve My Scar?
Although excision aims to create scars along natural skin creases and shadows, some scarring is inevitable. Here are tips to minimize their look and some treatments that may be offered:
Use sun protection (such as hats, long sleeves and pants, and sunscreen) and avoid tanning or burning around the scar if possible.
Keep the wound moist by covering it with Vaseline during wound healing.
Ask you dermatologist about the benefits of Silicone gel or sheets, which some dermatologists believe can help soften or flatten scars.
Camouflaging makeups or coverups can be used once your wound is healed but the scar has not fully formed.
An injection of a steroid solution may be offered if your scar is thicker than you prefer or is itchy long after surgery.
Procedures such as dermabrasion and laser surgery may be offered to help with the texture and color of your scar.
Minor surgical repair is very rarely necessary and will only be offered if there is considerable dissatisfaction and a high chance of improvement.
Your dermatologist can discuss suitable scar treatments to meet your needs and budget. More treatments are being developed every year to minimize scarring.
When is Excision Necessary?
In general, surgical excision may be warranted when:
Skin biopsy confirms a diagnosis of skin cancer and there is cancer remaining in the skin
An unusual mole, growth or spot looks highly suspicious for skin cancer
A lesion shows signs of changing or bleeding
Screening tests indicate melanoma risk factors are present
Previous non-surgical treatment didn’t successfully eradicate your skin cancer
Be cautious about self-diagnosis and always ask your dermatologist about a spot that worries you. They will then help you decide if a skin biopsy or excision is necessary. Catching skin cancers early can help minimize the health risks associated with cancer and the risk of complications after surgery.
Summary of Key Points
Surgical excision performed by a dermatologist is an extremely common outpatient technique to remove and diagnose various skin cancers.
The procedure is generally quick, safe and straightforward. While no surgery is completely without risks, excision proves highly effective for clearing margins and sparing healthy tissue when done properly.
Use the tips here to ease anxiety and optimize healing. With close follow up, most patients see excellent long-term outcomes from this precise approach.
-
What is elliptical excision?
Elliptical excision is a common surgical procedure used to remove skin lesions or skin cancers. The excision is generally performed in the shape of an ellipse, which looks similar to an oval or football.
What is Mohs surgery?
Mohs surgery is a specialized type of excision that allows for more precise removal of skin cancers on areas that are cosmetically sensitive or don’t have much excess skin, such as the face, hands, and genital area. It involves the removal of layers of cancer-containing skin, examining the tissue under a microscope during the procedure, and continuing the process of layered removal on the day of your procedure until no cancer cells remain. It is associated with higher rates of cure and improved cosmetic outcomes when used in the appropriate setting.
What is the role of a pathologist in dermatology?
Pathologists examine tissues and cells to diagnose diseases, including skin diseases and cancers, by analyzing samples of skin obtained during a biopsy or excision under a microscope.
What happens during a surgical procedure in dermatology?
A surgical procedure is a very broad term used in dermatology; it encompasses excision for skin cancer, but also includes many other treatments and procedures on the skin and other tissues.
Is general anesthesia used in dermatological procedures?
General anesthesia is a state of controlled unconsciousness during which you will be unaware and have no sensations or memories of the surgical procedure. It is typically not used in skin surgery, though there may be exceptions.
What are the precautions around the surgical site after a dermatological procedure?
After a dermatological procedure, it is important to allow the surgical site to heal properly. This may involve avoiding getting the surgical site wet, following the instructions provided by the dermatologist for advice, and watching for any redness, swelling, tenderness, or drainage.
What does the phrase 'surrounding tissue' mean in surgery?
The surrounding tissue refers to the adjacent or nearby tissue surrounding a specific area or organ, which may play a role in a medical condition or procedure.
How is the term 'topical' related to skin surgery?
Topical refers to medications or treatments applied directly to the skin surface. It can be used for pre- or post-operative care in excision of skin procedures or other excision surgery methods. Topical treatments may be part of treatment options for skin problems or forms of skin cancer.
What factors determine the type of excision surgery?
The type of excision surgery performed depends on various factors, including the size and depth of the area of skin involved, the need for skin graft or other reconstructive techniques, and the type of skin cancer, and most importantly the patient’s unique risk factors and medical history. For atypical moles, margins can vary greatly. For BCC and SCC, margins are typically 4 mm. For melanoma in situ, this margin can be 5 mm or more. For melanomas, this can vary depending on how advanced it is, but is generally as large as 1-2 cm.
When is a sentinel lymph node biopsy performed in skin excision surgery?
A sentinel lymph node biopsy may be performed to determine if forms of skin cancer have spread beyond the primary area of skin involved. This procedure involves injecting a dye or radioactive substance near the tumor site to identify lymphatic drainage. It is typically used for melanomas but can also be used for other types of cancers.
-
We are a group of dermatology residents and attending physicians based in Boston, MA. Our team of Ivy League-trained dermatologists is demystifying the cosmeceutical industry by offering unbiased, scientifically supported reviews of skincare products. We are extremely passionate about skincare and making it accessible to all through education. We value integrity, practicality, and inclusivity. No sponsorships were received for the products prior to testing; we feel strongly about providing un-biased reviews. After blogs are published, following the links in this blog post may result in commission.